Epilepsy & Functional Neurosurgery: Surgical Relief from Seizures and Movement Disorders
Advanced Brain Surgery at Vanchilingam
- Surgical options for drug-resistant epilepsy and disabling motor symptoms.
- Includes resective surgery, corpus callosotomy, laser ablation, and deep brain stimulation.
- Real-time EEG mapping and intraoperative monitoring for precise and safe interventions.
- Multidisciplinary planning with neurologists, neurosurgeons, and rehabilitation experts.
Epilepsy & Functional Neurosurgery: Advanced Surgical Solutions for Seizures and Movement Disorders
“When medications no longer work, precision surgery offers new hope.”
At Vanchilingam Advanced Neurology and Stroke Care, we offer specialized epilepsy and functional neurosurgery for patients whose seizures, tremors, or motor symptoms are not controlled by medications. These surgical interventions are designed to interrupt abnormal brain activity, restore control, and dramatically improve quality of life.
When Is Epilepsy or Functional Surgery Recommended?
Surgery is considered when:
- Seizures are drug-resistant (medication fails to control them)
- There is a clearly defined seizure focus in the brain
- Movement disorders (e.g. Parkinson’s, tremor) severely limit daily function
- Diagnostic imaging confirms that surgery can be performed safely
- Alternative neuromodulation techniques are insufficient

Conditions Treated with Surgery
- Drug-resistant epilepsy
- Parkinson’s disease
- Essential tremor
- Dystonia
- Tourette syndrome
- Cerebral palsy-related spasticity
- Hemifacial spasm or post-stroke movement disorders
Surgical Options We Offer
Resective Epilepsy Surgery
Surgically removes the seizure focus area-commonly used for temporal lobe epilepsy.
Offers high rates of seizure freedom or significant reduction.
Laser Ablation (LITT)
Minimally invasive technique using laser heat to destroy seizure-generating tissue.
Corpus Callosotomy
Cuts the connection between brain hemispheres to prevent seizure spread-used in generalized or drop seizures.
Responsive Neurostimulation (RNS)
Implanted device that detects seizure activity and disrupts it with electrical pulses.
Suitable for patients with deep or bilateral seizure foci.
Deep Brain Stimulation (DBS) Surgery
Electrodes are implanted in specific brain areas to manage Parkinson’s, dystonia, and tremors.
Motor Cortex Stimulation / Functional Mapping Surgeries
Used in advanced motor disorders, especially when exact brain function areas must be preserved.
Our Comprehensive Surgical Approach
- Video EEG monitoring and seizure mapping
- MRI, PET, and functional imaging (fMRI, DTI) for accurate localization
- Intraoperative brain mapping and neuromonitoring
- Multidisciplinary planning with neurologists, neuropsychologists, and rehab experts
- Tailored surgical plans based on your goals, symptoms, and safety profile
Why Choose Vanchilingam for Functional Neurosurgery?
- Fellowship-trained epilepsy and functional neurosurgeons
- Neuronavigation and intraoperative mapping to protect speech, movement, and memory
- Close collaboration with neurologists and rehab teams
- Access to advanced neuromodulation for patients not eligible for resective surgery
- Transparent counseling on risks, benefits, and life after surgery
Life After Surgery: What to Expect
- Patients may experience a significant drop in seizure frequency or tremor severity
- Hospital stay ranges from 2–5 days depending on the procedure
- Rehabilitation, medication tapering, and lifestyle guidance support long-term outcomes
- Ongoing follow-up with neurology and neurosurgery ensures progress tracking
Seizure Freedom Starts with Surgical Precision
For patients living with uncontrolled seizures or disabling movement disorders, surgery can be life-changing. At Vanchilingam Advanced Neurology and Stroke Care, our goal is to give you your life back-safely, confidently, and with expert care.
Contact us today to explore your eligibility for epilepsy or functional neurosurgery.
Meet the Specialists
Our team of dedicated specialists brings years of expertise and a passion for delivering personalized care.
Real Experiences, Real Results
Discover how Dr. Vanchilingam Advanced Neuro & Stroke Hospital has transformed the lives of our patients. Also hear our specialists talk about the services and solutions we offer for various neurological issues.




OUR SPECIALITY
Acute Stroke Unit
The Acute Stroke Unit is an acute neurological ward providing specialist services for people who have had a new suspected stroke. On the Acute Stroke Unit we provide: Thrombolysis treatment -treatment is started in the Emergency Department and you will have the rest of your Treatment and monitoring on the Acute Stroke Unit
OUR SPECIALITY
Advanced Neuro ICU
A neuro ICU is an Intensive Care Unit which is particularly devoted to a high – quality care of patients with the neurological problems that are life-threatening in nature. The neuro ICU of our hospital is a complete state of the art and a full-fledged one designed to provide almost all sorts of advanced neurological care to the normal patients as well as the patients in the emergency.
OUR SPECIALITY
Advanced Neuro Imaging
Our radiology department is a state of the art department with all the necessary infrastructure that is essential for effectively dealing with the neuro and neurosurgery emergencies at its best. The advanced neuroimaging techniques used by our doctors are as discussed below.
OUR SPECIALITY
Neuro interventional Cath Lab
A neuro-interventional Cath lab in a neurodiagnostic Centre is a specialized catheterization laboratory which has all the necessary diagnostic imaging equipment that is particularly used for the purpose of visualization of the arteries, veins and other vascular malformations of the brain and spinal cord.
OUR SPECIALITY
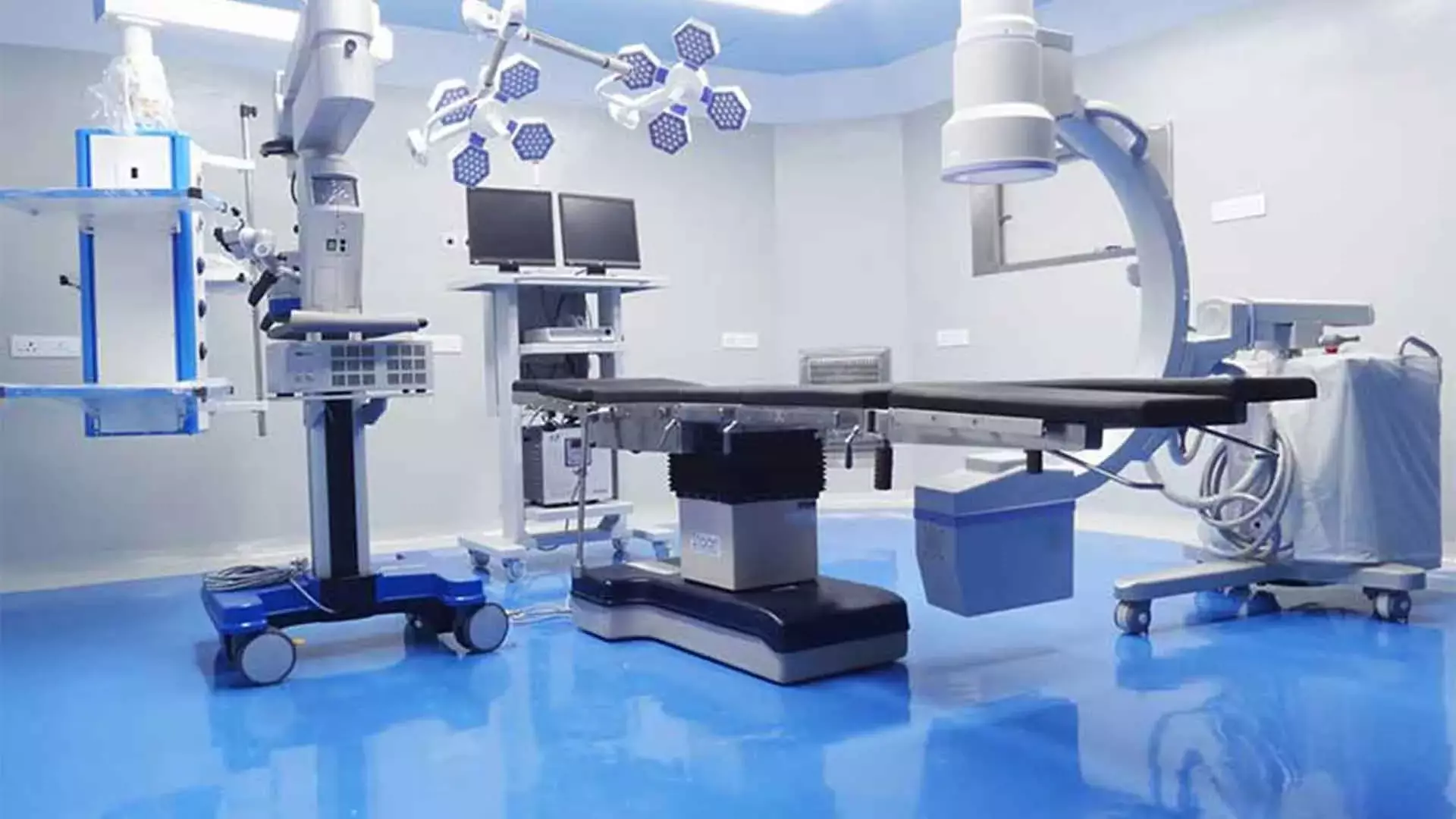
Neuro-Surgery Operating Room
The neurosurgery operating room of Dr.Vanchilingam Hospital, Neurosurgery Hospital is a fully functional and a state of art one that has the adequate infrastructure for effectively carrying out even the most complicated neuro surgeries with ease.
What is epilepsy and functional neurosurgery?
Epilepsy and functional neurosurgery refers to specialized brain surgeries aimed at treating drug-resistant seizures and disabling motor disorders such as Parkinson’s disease and dystonia. These procedures target specific brain areas to restore normal function.
When is epilepsy or functional surgery recommended?
Surgery is considered when seizures are drug-resistant, there is a clear seizure focus in the brain, or when motor symptoms severely affect daily life. It’s also considered if diagnostic imaging shows the procedure is safe and neuromodulation hasn’t worked.
Which conditions can be treated with epilepsy and functional neurosurgery?
Conditions treated include drug-resistant epilepsy, Parkinson’s disease, essential tremor, dystonia, Tourette syndrome, cerebral palsy-related spasticity, and post-stroke movement disorders.
What surgical options are available for epilepsy and functional neurosurgery?
We offer resective epilepsy surgery, laser ablation (LITT), corpus callosotomy, responsive neurostimulation (RNS), deep brain stimulation (DBS), and motor cortex stimulation.
How does resective epilepsy surgery help patients?
This procedure removes the seizure focus in the brain, often used for temporal lobe epilepsy, and can lead to seizure freedom or significant reduction.
What is laser ablation (LITT) in epilepsy treatment?
Laser ablation is a minimally invasive procedure that uses targeted heat to destroy seizure-generating tissue with precision.
What is corpus callosotomy and when is it used?
Corpus callosotomy involves cutting the connection between brain hemispheres to prevent seizure spread, commonly used in generalized or drop seizures.
How does responsive neurostimulation (RNS) work?
RNS involves implanting a device that detects and disrupts seizure activity using electrical pulses, suitable for deep or bilateral seizure foci.
What is deep brain stimulation (DBS) used for?
DBS involves placing electrodes in the brain to manage conditions like Parkinson’s disease, essential tremor, and dystonia.
What should patients expect after surgery?
Patients often see reduced seizure frequency or tremor severity. Hospital stay is usually 2–5 days, followed by rehabilitation, medication adjustments, and long-term follow-up with specialists.











